Perfusion Without Borders – Scholarship Winner
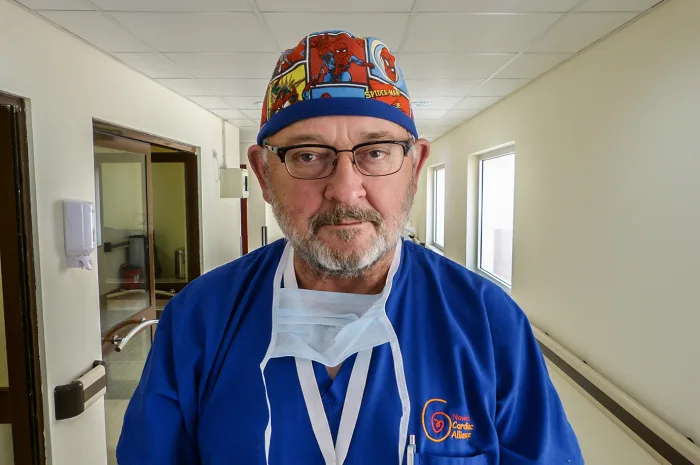
Each year, the American Society of Extracorporeal Technology offers a scholarship to one Perfusion student to travel on a medical mission trip with an organization of their choice. This year’s winner is perfusion student Amy Evans and she will be traveling with Novick Cardiac Alliance to Ukraine in December 2018. Amy Evans is currently a …